AIHW Mothers and Babies report
- maternityconsumer
- Sep 25, 2024
- 3 min read
Here is a quick summary of the National Mothers and Babies report, by Edwina Mead from our Committee:
MCN has been focusing on roadside births lately (0.9%), as this is a result of declining number of regional maternity services. Similarly, I note in this report that:
remote/very remote women were less likely to receive antenatal care in the first trimester (71%/67%) compared to the national average of 78%. This is much the same as last year, where interestingly inner regional women were most likely, followed by outer regional, then major cities, then remote, and finally very remote.
Remote women were less likely to have received at least 5 antenatal care visits during pregnancy (89%) compared to average 94%. Inspecting last year's data showed that the more remote the residential, the less likely the woman was to have 5+ visits.
Babies born to Very remote mothers were more likely to have a hospital stay longer than 6 days (14%). No average is given, but only 2.9% of term babies did the same. Looking at last year's report, the number of babies staying >6 days does indeed increase with remoteness (5.9% major cities/inner regional, 6.9% outer regional/remote, 8% very remote). There is no explanation given on why this might have increased so much year on year.
The chart isn't available in the preview, but I note in last year's report (and see no reason why it would have changed) that the proportion of low birth weight and preterm babies increases with remoteness; similarly admission to special care or neonatal ICU increases by remoteness (except for "remote" 🤷♀️)
For the second time in history, less than half of women (49%) had a spontaneous vaginal birth (no caesarean and no instrumental assistance, but may have been induced or augmented).
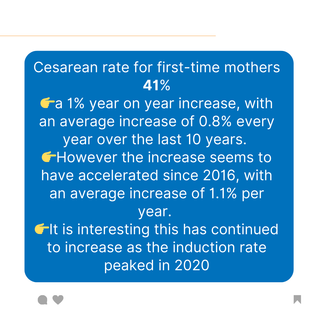
I also note that the CS rate for first-time mothers is now 41%, a 1% year on year increase, with an average increase of 0.8% every year over the last 10 years. However the increase seems to have accelerated since 2016, with an average increase of 1.1% per year. It is interesting that this has continued to increase as the induction rate peaked in 2020 (and induction is known to increase the CS rate, particularly for first-time mums).
Mothers over 35 had a caesarean section rate of 49%. This is a 1.4% increase year on year, which is a pretty big jump given the average increase has been less than 0.5% per year since 2011. This is quite strange - Alecia, do you know of any policy changes that may have been driving this?
The rate of spontaneous labour is now only 41% for all women, and of these, 27% had augmentation of labour (labour sped up with drugs). This means that only 30% of all women laboured without the use of drugs to start or speed up labour. There is not sufficient data reported to understand how augmentation affects the rate of instrumental or caesarean birth, but assuming it doesn't change the rate (unlikely!) then only 21% of women have a spontaneous labour with no augmentation resulting in a spontaneous vaginal birth. If you add in episiotomy, and again, there's not enough information to understand the effect of induction OR augmentation, but taking the average rate, only 18% make it through without being cut. There's no data reported on drugs given as part of managing the birth of the placenta. I suspect it's quite high, since that is routine practice in hospital. Now that's pretty dismal odds of having a no/low intervention birth!
Still no change in the rate of normal birth weight for Indigenous babies (88%, same as last year, compared to 87.8 in 2014).















Comments